After experiencing gender dysphoria from age 6, Patient X is referred at age 14 years to the gender identity service by their GP.
Read the patient information and consider the questions below.
Patient X was referred via their general practitioner (GP) to the gender identity service for long-standing gender identity issues. The patient is now aged 14.5 years and the gender dysphoria was reported by parents from the age of 6 years.
Patient X was accepted by the gender identity service and diagnosed with gender dysphoria using the Diagnostic and Statistical Manual of Mental Health Disorders (DSM-5-TR). The DSM-5-TR defines gender dysphoria in children as a marked incongruence between one’s experienced/expressed gender and assigned gender, lasting at least 6 months, as manifested by at least six of the following features (one of which must be the first criterion):
- A strong desire to be of the other gender or an insistence that one is the other gender (or some alternative gender different from one’s assigned gender);
- In boys (assigned gender), a strong preference for cross-dressing or simulating female attire; or in girls (assigned gender), a strong preference for wearing only typical masculine clothing and a strong resistance to the wearing of typical feminine clothing;
- A strong preference for cross-gender roles in make-believe play or fantasy play;
- A strong preference for the toys, games or activities stereotypically used or engaged in by the other gender;
- A strong preference for playmates of the other gender;
- In boys (assigned gender), a strong rejection of typically masculine toys, games and activities, and a strong avoidance of rough-and-tumble play; or in girls (assigned gender), a strong rejection of typically feminine toys, games, and activities;
- A strong dislike of one’s sexual anatomy;
- A strong desire for the physical sex characteristics that match one’s experienced gender.
As with the diagnostic criteria for adolescents and adults, the condition must also be associated with clinically significant distress or impairment in social, occupational, or other important areas of functioning.
They were offered on-going support on an annual basis but at the time of puberty the gender dysphoria became very difficult for Patient X.
Following all appropriate assessments by a psychologist, and in agreement with the multidisciplinary team and the NHS England multiprofessional review group, a referral was made to the paediatric endocrinology team. The referral was triaged and accepted as appropriate.
Nurse-led Education Session – Initial Appointment
The nurse-led education session is run by clinical nurse specialists and provides both the young person and their family important information on what our service can offer, options for treatment, reasons for smoking cessation, fertility preservation, bone health, sexual health and vitamin D supplementation. We have produced an extensive information pack which is provided to take away. Baseline tests are undertaken at this initial appointment to prevent repeated trips and additional cost as many of our families travel long distances to attend clinic. This also allows for all results to be available for the first consultant appointment, thus improving patient satisfaction. If it has been identified that the group session is inappropriate for the young person, then the initial appointment will be with the consultant paediatric and adolescent endocrinologist.
Baseline tests
Blood tests include urea and electrolytes, liver function tests, cholesterol, ferritin, 17-hydroxyprogesterone, dehydroepiandrosterone sulphate, follicle-stimulating hormone, luetenising hormone, thyroid function tests, parathyroid hormone, testosterone, oestrogen and vitamin D. Dual X-ray absorptiometry (DEXA) should be performed.
Patient X was found to be vitamin D deficient and a treatment course was prescribed by the GP. All other investigations were within normal parameters.
Figure 1. The hypothalamic–pituitary–gonadal axis negative feedback loop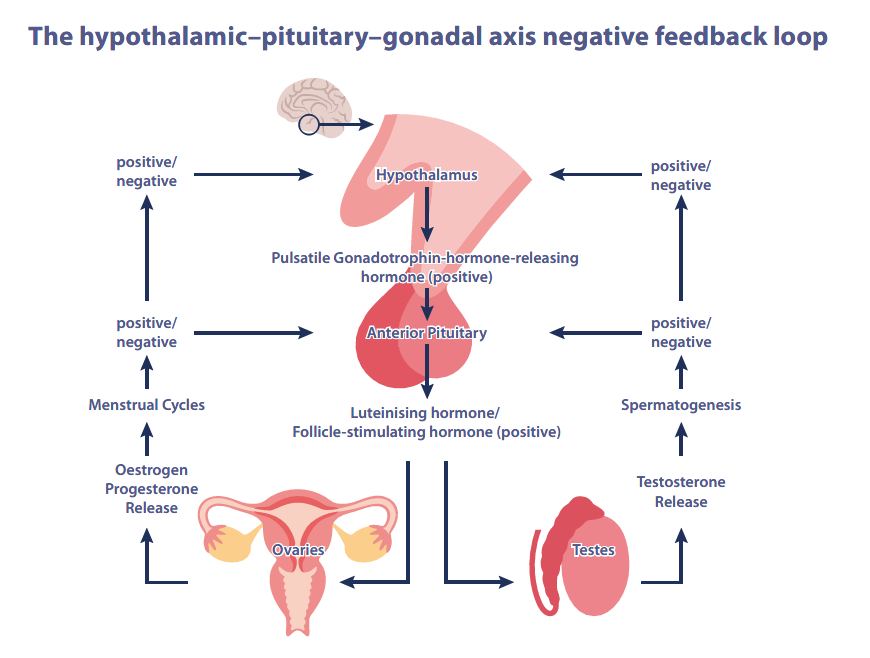
Legend: The hypothalamus releases gonadotropin-releasing hormone which is transported to the anterior pituitary and binds to the GnRH receptor. This leads to production and secretion of luteinising hormone and follicle-stimulating hormone. These gonadotropins enter the blood stream and binds to a receptor in the gonads, stimulating secretion of sex steroids, androgens and oestrogens for regulation of the menstrual cycle or spermatogenesis.
Endocrinologist Appointment
The young person along with their family are invited back around 2 months after the nurse-led education session to meet the endocrinologist at a multidisciplinary clinic. This is also attended by the clinical nurse specialist along with a member of the psycho-social team.
It is made clear that before being considered for any medical interventions, it is important to undertake several assessments. This ensures that starting medication is the right choice for the young person and allows the assessment and explanation of the effects of any medication the young person may receive. This will include a medical history, feedback on earlier baseline tests, height, weight and a physical examination to check general health and pubertal development.
If the medical treatment option is agreed, then consent will be taken from the young person/parent along with the endocrinologist. GnRH analogues (sex hormone blocker) are used for at least 12 months to pause puberty to alleviate any distress regarding physical changes to the body as well as providing further space for exploration with the psycho-social clinician.
Treatment Plan
Patient X was assessed by their endocrinologist to determine whether they had the maturity and understanding to consent to treatment (Gillick competency) and parental consent was taken and this was signed by the endocrinologist. It was agreed by all professionals involved that treatment with GnRH analogues would be in Patient X’s best interests. The GP was written to with the advice to commence prescribing of gonapeptyl 3.7 mg to be administered via intramuscular injection every 28 days. If this is tolerated the prescription can be changed to decapeptyl 11.25 mg via intramuscular injection every 10 weeks.
Monitoring
It is essential that Patient X continues to have regular follow-up appointments with their psycho-social clinician alongside 6-monthly endocrine appointments with a clinical nurse specialist or an endocrinologist. Blood tests will be taken every 6 months to check hormonal suppression and a DEXA scan will be undertaken every 12 months to monitor bone health. Patient X will be required to attend all these appointments so physical and emotional health can be monitored on a regular basis.
Gender Affirming Hormones
After a minimum of 1 year on GnRH Analogues, and not before 16 years of age, gender affirming hormones may be commenced. If appropriate, Patient X will be required to have met with their psycho-social clinician on a regular basis to complete their assessment and discuss the option of introducing gender affirming hormones.
Once a full assessment by the psycho-social team has been undertaken and informed consent has been obtained by the endocrinologist then the young person may commence testosterone or oestrogen.
Gender affirming hormones are prescribed as per the NHS adolescent treatment schedule.
Oestrogen (male to female / trans female) (Generally continue GnRHa throughout)
Estradiol valerate: tablets strength: 1 mg and 2 mg available: Maximum dose: 6 mg/day
- Can titrate by 1–2 mg at 6-month intervals (depending upon clinical response & oestradiol levels)
- Aim for young adult female levels of 400–600 pmol/L when on established adult doses
Testosterone (female to male / trans male)
Depot testosterone : Can be given concomitantly with GnRHa.
- GnRHa will be withdrawn once adult male testosterone levels are achieved
- Depot testosterone is titrated at 6-month intervals on a case by case basis
| Dose level 1 | Depot testosterone | 100 mg (0.4 mL) | Intramuscular | Every 4 weeks |
| Dose level 2 | Depot testosterone | 200 mg (0.8 mL) | Intramuscular | Every 4 weeks |
| Dose level 3 | Depot testosterone | 250 mg (1 mL) | Intramuscular | Every 4 weeks |
Summary
- Patient X attended the gender identity service at age 14.5 years with long-standing gender identity issues and was found to meet DSM-5-TR criteria for gender dysphoria.
- A referral was made to the paediatric endocrinology team for an initial appointment with an endocrine nurse and baseline blood and bone density tests.
- Patient X subsequently had a meeting with the endocrinologist, endocrine nurse and a member of the psycho-social team to discuss general health and medical interventions.
- Patient X was assessed for ability to give consent to treatment, in agreement with their parents, and received a prescription for a depot GnRH analogue to pause puberty for at least 12 months.
- Patient X will continue with regular psycho-social and endocrine nurse appointments to monitor physical and emotional health during treatment.
- One year or later, patient X may be assessed for the introduction of gender affirming hormone therapy.
Key learning points
- Children with gender identify concerns may be referred by their GP to the gender identity service and diagnosis is made using the DSM-5-TR criteria.
- Following psychological assessments, the child may be referred to the paediatric endocrinology team for an endocrine nurse-led session on service provisions and baseline health testing.
- The adolescent may be considered by an endocrinologist for puberty blocking therapy with a GnRH analogue, lasting at least 1 year.
- The adolescent may be subsequently considered for gender affirming hormone therapy.
- The adolescent should be regularly assessed throughout by DEXA scanning for bone density and hormone levels, and by the psycho-social team for consent and emotional health.



