A boy called “Ivan” aged 15 years and 9 months is referred to the endocrine clinic by his newly appointed GP following his concerns regarding delayed puberty.
Read the patient information and answer the questions below.
Question 1.
What is the definition of delayed puberty?
- Boys who show no increase in testicular volume of >3 mL by age 14; Girls without breast development by age 13 or girls with breast development but without menstruation by age 15
- Boys or girls who start secondary school without any signs of pubertal development
- Boys who fail to complete puberty by age 18 years; Girls who fail to complete puberty by age 16 years
Boys who show no increase in testicular volume of >3 mL by age 14; Girls without breast development by age 13 or girls with breast development but without menstruation by age 15.
Presenting complaint
- Ivan and his family had concerns surrounding his lack of pubertal development
- Ivan with the support of his mother initially sought the opinion of a paediatrician in their home country of Slovenia
- After initial investigations, he was started on testosterone treatment
Early history
- Born at term by a standard vaginal delivery
- Mother reports concerns after birth surrounding neonatal asphyxiation and subsequent seizures, required a 1-month stay in the neonatal intensive care unit
- After regular follow up, he was discharged
- Normal growth and cognitive development reported after that, with no ongoing concerns
Past medical history
- Undescended left testis removed aged 6 months, during orchidopexy only a testicular remnant identified
Family history
- Younger brother has beta thalassaemia trait
- No parental consanguinity
- No other family history of note
Medication history
- Started on testosterone replacement therapy (TRT) in home country at age 15 years 7 months
- Two doses of 50 mg of testosterone enanthate administered intramuscularly (im) 4 weeks apart
- Third injection 50 mg im given by healthcare professional in the UK
- Subsequent injections increased to 100 mg every 4 weeks to be administered at GP practice
- No known drug allergies
- Up to date with all immunisations
Social history
- Lives at home with his mother, father, and younger brother
- In year 11 at school, doing well
- Enjoys playing basketball with his friends
Systems Review
- No headaches
- No vision changes
- Normal sense of smell
- No nausea or vomiting
- No unintentional weight loss
- No diarrhoea
Overall
- Patient is alert, talking, and appears well
- Phenotypically male with no dysmorphic features identified
- Cardiovascular System: warm and well perfused; Heart sounds I+II present with no added sounds
- Respiratory System: no signs of respiratory distress
- Musculoskeletal system and skin: no joint swelling, no deformities, no rashes
- Abdominal: Soft non tender with no palpable masses
Anthropometrics
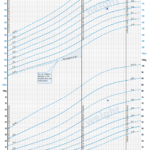
- Age – 15 years and 9 months
- Height – 171.4 cm (standard deviation score [SDS] –0.14)
- Height centile – between 25th and 50th centile
- Mid parental height target – 50th centile
- Weight – 72.5 kg
- Weight centile – between 75th and 91st centile
- BMI – 24.68 kg/m2 (SDS +1.6)
Tanner staging
- Tanner stage of pubic hair – P3
- Tanner stage of axillary hair – A2
- Left testis absent
- Right testis small 1–2 mL and very soft
- Penis length 6 cm with good width
- No facial hair
- No acne
Question 2.
From the history and examination findings, what initial investigations would you like to carry out?
- Serum follicle stimulating hormone (FSH) and luteinising hormone (LH), Serum testosterone, Magnetic resonance imaging (MRI) of the pelvis, Karyotyping
- MRI brain, Pelvic ultrasound, Serum prolactin
- Gonadotrophin-releasing hormone stimulation test, Karyotyping, Computed tomography of the adrenals
Serum follicle stimulating hormone (FSH) and luteinising hormone (LH), Serum testosterone, Magnetic resonance imaging (MRI) of the pelvis, Karyotyping
| Full blood count | Results (reference ranges) |
|---|---|
| Haemoglobin (Hb) | 132 g/L (130–170) |
| White blood count (WCC) | 8.8 x 10^9/L (4–10) |
| Platelet count | 276 x 10^9/L (150–410) |
| Haematocrit | 0.4 (0.4–0.5) |
| Red blood count | 4.53 x10^12/L (4.5–5.5) |
| Mean cell volume (MCV) | 89 fL (83–101) |
| RBC distribution width | 13.3% (11.6–14) |
| Mean cell haemoglobin | 29.1 pg (25–33) |
| Mean cell haemoglobin concentration | 328 g/L (315–345) |
| Neutrophil count | 5.3 x10^9/L (2–7) |
| Lymphocyte count | 2.4 x10^9/L (1–3) |
| Monocyte count | 1.0 x10^9/L (0.2–1) |
| Eosinophil count | 0.1 x10^9/L (0–0.5) |
| Basophil count | 0.1 x10^9/L (0–0.1) |
| Nucleated RBC count | 0.0 x10^9/L (0–0.2) |
| Immature Granulocytes | 0.1 x10^9/L (0–0.3) |
| Urea and electrolytes | |
| Sodium | 140 mmol/L (133–146) |
| Potassium | 4.7 mmol/L (3.5–5.3) |
| Chloride | 104 mmol/L (95–108) |
| Urea | 4.4 mmol/L (2.5–6.5) |
| Creatinine | 48 micromol/L (40–68) |
| Total Bilirubin | 7 micromol/L (0–21) |
| Liver function tests | |
| Alanine aminotransferase (ALT) | 24 units/L (0–41) |
| Alkaline phosphatase (ALK) | 228 unit/L (60–425) |
| Total Protein | 76 g/L (60–80) |
| Albumin | 47 g/L (35–50) |
| Calcium | 2.38 mmol/L (2.2–2.7) |
| Adjusted Calcium | 2.24 mmol/L (2.2–2.6) |
| Inorganic Phosphate | 1.75 mmol/L (0.9–1.8) |
| Lipid panel | |
| Total Cholesterol | 3.9 mmol/L (0–5) |
| LDL Cholesterol | 2.0 mmol/L (<3.0) |
| HDL Cholesterol | 1.6 mmol/L (0.9–1.5) |
| Triglycerides | 0.57 mmol/L (0–1.7) |
Endocrinology Blood Results (patient aged 15 years and 9 months)
| Follicle stimulating hormone (FSH) | 48.4 unit/L (1.5–12.4) |
|---|---|
| Luteinising hormone (LH) | 19.4 unit/L (1.7–8.6) |
| Oestradiol | <19 pmol/L (95–223) |
| Testosterone | 0.9 nmol/L (8.6–29) |
| Anti-Müllerian hormone (AMH) | <0.2 pmol/L (301–1015) |
| Inhibin B | <9.8 pg/ml (74–470) |
Previous results from home country (patient aged 15 years and 3 months)
| Follicle stimulating hormone (FSH) | 57 unit/L (1.5–12.4) |
|---|---|
| Luteinising hormone (LH) | 16 unit/L (1.7–8.6) |
Question 3.
From reviewing the blood results, what is now your top differential for ‘Ivan’s’ delayed puberty?
- Delayed puberty as a result of an undiagnosed chronic disease
- Kallmann Syndrome
- Pituitary lesion
- Primary gonadal failure
- Partial androgen insensitivity syndrome
Primary gonadal failure
Question 4.
Why are Ivan’s serum gonadotrophins elevated?
- Excessive uncontrolled production of gonadotrophins (FSH and LH) by a pituitary adenoma
- Lack of testosterone by the non-functioning testes imposes a lack of negative feedback exerted on the gonadotrophic cells of the anterior pituitary resulting in elevated serum FSH and LH
- Ectopic production of FSH and LH from a yet unknown source
Lack of testosterone by the non-functioning testes imposes a lack of negative feedback exerted on the gonadotrophic cells of the anterior pituitary resulting in elevated serum FSH and LH
Question 5.
What cells are responsible for the production of Inhibin B and what is its primary role in the HPG axis of males?
- Inhibin B is produced by the Sertoli cells; it acts to upregulate expression of testosterone receptors
- Inhibin B is produced by Sertoli cells; it acts to inhibit FSH from the anterior pituitary (an example of negative feedback)
- Inhibin B is produced by the Leydig cells, it acts to promote spermatogenesis
Inhibin B is produced by Sertoli cells; it acts to inhibit FSH from the anterior pituitary (an example of negative feedback)
Further investigations completed
Karyotype – 46 XY
MRI Pelvis – concluded normal male internal structures with no evidence of Müllerian structures (ovaries or uterus)
The patient’s perspective – Ideas, concerns, and expectations
Ideas
- ‘Ivan’ understands that he will require TRT lifelong
- He understands that his remaining left testicle has not developed properly
Concerns
- ‘Ivan’ is worried about his lack of pubertal development in comparison to his peers
- Reports feeling self-conscious about having one testicle
- Saddened to hear that his remaining testicle appears to not be functioning which will likely impede his ability to have children
- Continuation of testosterone injections to be delivered locally at GP practice, with a gradual increase of dose to induce pubertal characteristics
- Follow up at the paediatric endocrine clinic in ~4 months’ time
- To be contacted by the paediatric urology team regarding testicle prosthesis
Management
- Regular consultations in the paediatric endocrine clinic
- TRT in the form of testosterone enanthate 100 mg im – to be continued every 4 weeks, administered at GP surgery. This will then be gradually titrated up over the next 1–2 years to induce pubertal characteristics. Aiming to achieve an adult maintenance dose of 250 mg 4 weekly
- Patients on TRT require monitoring of haematocrit and haemoglobin – every 3 months for the first year, annually thereafter. Why? Severe polycythaemia is a rare but known side effect of TRT
- Baseline bloods to be repeated to assess treatment efficacy
- Disorders of sexual development (DSD) genetic panel to be completed
- When the times comes, transfer of care to an adult endocrinologist, ideally one with experience of male reproductive health
- Gradual transition to adult services will be required to ensure maintained patient compliance and ongoing support
- It is very unlikely that ‘Ivan’ will be able to conceive his own children; therefore, counselling around fertility should be offered in later life
- ‘Ivan’ will require lifelong TRT. Management of chronic conditions imposes various challenges to patients, therefore practical advice and psychological support should be offered
Question 6.
What possible side effects should a patient be advised about when starting TRT?
- Weight gain, hot flushes, and mood changes
- Nausea and vomiting, visual disturbances, dizziness
- Erectile dysfunction, weight loss, skin hyperpigmentation
Weight gain, hot flushes, and mood changes
Summary
- ‘Ivan’ has delayed puberty but is phenotypically male
- Baseline biochemistry demonstrates hypergonadotropic hypogonadism – high FSH and LH combined with low testosterone, low inhibin B, and low anti-Müllerian hormone suggestive of primary gonadal failure likely caused by gonadal dysgenesis
- Management of ‘Ivan’s’ primary gonadal failure will require lifelong TRT
- The aetiology of ‘Ivan’s’ poor testicular development is not yet understood – is this congenital, acquired, or multifactorial? DSD panel may provide some insight
Key learning points/conclusions
- Gonadal dysgenesis covers a spectrum of disorders, ranging from Swyer syndrome –in which a patient has an 46XY karyotype but is phenotypically female so therefore typically raised as a girl – to a milder phenotype as demonstrated by this case study
- This patient is phenotypically male (he does not have ambiguous genitalia) revealing that he must have had adequate exposure to testosterone to achieve testicular function both in utero and in early infancy
- In an 46XY foetus, normal foetal testicular function is required for the development of male external genitalia and the suppression of Müllerian structures
- This patient had no female reproductive organs detected on MRI pelvis revealing in early foetal development there must have been adequate anti-Müllerian hormone to ensure regression of the Müllerian ducts
- Anti-Müllerian hormone and Inhibin-B are peptide hormones which in males are produced by the Sertoli cells of the testes. ‘Ivan’s’ low levels of anti-Müllerian hormone and inhibin B are suggestive of poor development of the Sertoli cells, germ cells and seminiferous tubules of the testes
- It is important to manage the patient expectations. Following initiation of TRT ‘Ivan’ was pleased that aspects of his sexual function had improved, specifically that his “dry ejaculates” had now become more liquid, however was saddened to hear this did not mean sperm production was occurring
Extra information for interest
Causes of delayed/absent puberty
| Functional (intact HPG axis) | Hypergonadotropic Hypogonadism (High FSH/LH, low sex steroid hormones) | Hypogonadotropic Hypogonadism (Low FSH/LH, low sex steroid hormones) |
|---|---|---|
| Constitutional delay | Acquired gonadal failure | Acquired causes |
| Underlying chronic disease (cystic fibrosis, IBD, coeliac disease, malignancy etc) | Testicular or ovarian torsion | Benign tumours – craniopharyngioma, prolactinoma |
| Malnutrition | Iatrogenic (chemotherapy or radiation exposure, iron overload from repeated transfusions) | Infiltrating process: histiocytosis, granulomas, sarcoidosis or haemochromatosis |
| Excessive exercise | Consequence of drug or toxin exposure | Head injury (including birth hypoxia) |
| Anorexia nervosa | Viral infections (such as mumps or TB) | Iatrogenic (cerebral surgery or radiotherapy) |
| Prolonged stress – trauma, child abuse, war | Autoimmune | Stroke |
| Infiltrating process: granulomas, amyloidosis | Central nervous system infections | |
| Congenital gonadal failure | Congenital causes | |
| Chromosomal disorders – Klinefelter syndrome (47 XXY) or Turner Syndrome (45 X) | Kallmann syndrome (gonadotropin-releasing hormone [GnRH] deficiency associated with anosmia) | |
| Gonadal dysgenesis – including Swyer syndrome (XY gonadal dysgenesis), XX gonadal dysgenesis, as well as milder phenotypes | Isolated GnRH deficiency with normal sense of smell | |
| Androgen insensitivity syndrome – partial or complete | Loss of function mutation in neuropeptides such as kisspeptin, neurokinin B or their receptors | |
| Testicular regression syndrome | Hypopituitarism | |
| Gonadotropin resistance – such as Leydig cell hypoplasia in males or FSH insensitivity in females | Leptin deficiency | |
| Biosynthetic defects such as congenital adrenal hyperplasia | Syndromic, such as Prader–Willi Syndrome, Noonan Syndrome |
References for table
[1] [2]
What is a genetic testing panel?
A genetic testing panel is a single laboratory test, requiring a sample of patient blood or saliva, that looks for the presence of specific gene variants in multiple genes that are known to be associated with a specific syndrome or condition.
What are disorders of sexual development (DSD)?
A group of congenital conditions associated with atypical development of chromosomal, gonadal and/or phenotypic sex. It is a highly heterogeneous group of disorders, which range in severity from simple hypospadias in boys, to full XX or XY sex reversal.
What is a DSD panel?
It is a genetic panel that can be used to analyse whole genome or exome data of patients identified with a DSD. According to Genomics England, the panel was originally developed for the 100,00 Genomes Project but it is regularly being reviewed and updated to reflect new findings. Currently, the panel consists of 69 genes whose variants have been identified to be associated with a DSD. Each gene is given a rating dependent on the currently available evidence, with those labelled “green” having high evidence, those labelled “amber” having moderate evidence, and those labelled “red” having low evidence.
It is currently known that only 13% of patients identified with a DSD receive an accurate genetic diagnosis [3]. Therefore, the aim of this panel is to improve this statistic, achieve a genetic diagnosis, and ultimately improve the management of these patients. Finding a diagnosis also helps to identify risk of long-term outcomes, as well as informing families who may require genetic counselling [4].
Click here to go to view the DSD panel used by NHS England