Case history
Three-week-old baby referred to the paediatric endocrine clinic from a general paediatrician with ambiguous genitalia, accompanied by very anxious and upset parents.
Previous history
Early history
- Only child
- Non-consanguineous parents
- No family history of DSD (differences in sex development)
- No family history of unexplained neonatal deaths
- Born at term
- Normal vaginal delivery
- Weight 4.53 kg
- Clinically well
History
Health and medication history
- Antenatal ultrasound showed external genital appearance consistent with a boy
- Parents decorated the nursery in blue and had bought “boy” toys and clothes
- Male sex of rearing assigned at birth
- Given a male name
- Postnatal baby check revealed no testes in the scrotum
Question 1.
What would the immediate differential diagnoses be?
- Hypospadias (male infant)
- Cryptorchidism (male infant)
- Anorchia (male infant)
- Ambiguous genitalia
- Virilised congenital adrenal hyperplasia (female infant)
Question 2.
Which genitalia rating scale would be most useful during the clinical examination?
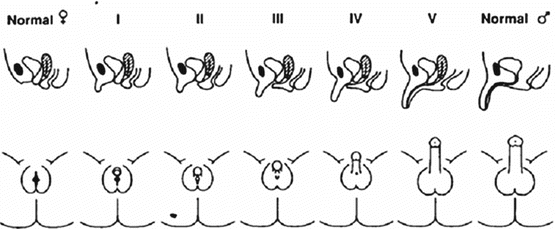
- Prader scale
- Quigley Scale
- External masculinisation score (EMS)
Prader scale
Question 3.
Which initial urgent biochemical investigations would you want to undertake?
- U&E (urea and electrolytes)
- Blood glucose
- FISH (fluorescence in-situ hybridisation), to identify the presence of Y chromosome material
- Karyotype
Question 4.
What other biochemical investigations would you subsequently want to undertake?
- Luteinising hormone
- Full blood count
- Cortisol
- 11-Deoxycortisol
- Bone Profile
- Follicle-stimulating hormone
- Plasma renin activity
- Aldosterone
- Human chorionic gonadotropin
- 17-hydroxyprogesterone (17-OHP)
- Androstenedione
- Urine steroid profile
- Testosterone
- Anti-Müllerian hormone
- Inhibin B
- Cortisol
- 11-Deoxycortisol
- Plasma renin activity
- Aldosterone
- 17-hydroxyprogesterone (17-OHP)
- Androstenedione
- Urine steroid profile
- Testosterone
- Anti-Müllerian hormone
- Inhibin B
Question 5.
What other investigations would be useful?
- Laparoscopy
- Clinical photography
- Gonadotropin-releasing hormone test
- Urinalysis for proteinuria
- Corticotropin-releasing hormone test
- Pelvic ultrasound
- Insulin tolerance test
- Bloods for DNA storage
- Parental bloods for DNA
- Synacthen test
- Combined pituitary function test
- Micturating cystourethrogra
- Clinical photography
- Urinalysis for proteinuria
- Pelvic ultrasound
- Bloods for DNA storage
- Parental bloods for DNA
- Synacthen test
Results of investigations
Prader V on Prader virilisation scale (marked virilisation of the external genitalia)
Increased urinary steroid profile
46, XX Karyotype
17-OHP – 101.9 nmol/L (normal range 0–5 nmol/L)
Ultrasound scan – Normal bladder and kidneys, ovaries present
Question 6.
What is the definitive diagnosis?
- Female infant 46
- XX with 21-Hydroxylase Congenital Adrenal Hyperplasia
Question 7.
Who do you think are the key personnel of the multidisciplinary team that should be involved with this baby and their family?
- Paediatric Endocrinologist
- Clinical Nurse Specialist
- Paediatric Urologist
- Psychologist
Question 8.
What is the management plan for this baby?
- Commence hydrocortisone, fludrocortisone and additional salt supplements in feeds.
- Intensive “sick-day management” education from the Clinical Nurse Specialist, including doubling up of hydrocortisone and emergency hydrocortisone injections.
- Gender assignment: reassignment to female gender was recommended.
- Close liaison with general practitioner and community nursing teams for regular (every 2 weeks to start with) for bloods for sodium and 17-OHP levels, and management of repeat prescriptions.
- Involvement with psychology services.
- Genetic counselling: the risk of subsequent affected infants is one in four for each infant.
Conclusion
This baby required intensive medical and psychological management, as well as high-level nursing intervention. The parents remained anxious, including the father who was very angry as he felt he had “lost” a son, and blamed the medical team. However, the full multidisciplinary team approach was mandatory, and was fully supportive and understanding of the parental needs. The baby and family are now thriving in the paediatric endocrine clinic.



